


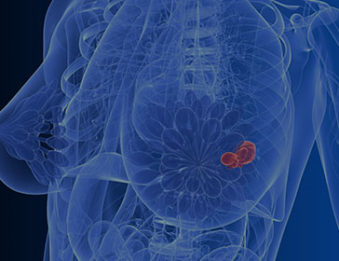
Breast cancer begins when the cells in the breast grow rapidly and out of control and form a tumor, or lump, in the breast. In most cases, the abnormal growths show up on a screening mammogram as a new shadow or cluster of microcalcifications. Although breast cancer can occur in men, 99% of all breast cancers occur in women. Breast cancer usually grows from the ducts that carry the milk to your nipple. Some cancers grow from the lobular ducts that make breast milk. More women are diagnosed with breast cancer than any other type of cancer.
If you’ve been diagnosed with breast cancer, our board-certified radiation oncologist will work with your medical team to discuss the array of advanced treatment options available to you and the success rates with each type.
Some factors may increase your risk of getting breast cancer. Somewhere between five and ten percent of cancers are inherited from changing genes that are passed down within a family. Most women diagnosed with cancer have no family connection and no obvious risk factors. Although most breast cancers might appear to occur by chance, radiation oncologists have outlined some lifestyle factors they believe may increase your risk of breast cancer.
Lifestyle Factors:
 Mat-Su Valley Cancer Center is one of the premier facilities in Alaska with the most advanced technology and unsurpassed expertise to manage and treat all types of breast cancer.
Mat-Su Valley Cancer Center is one of the premier facilities in Alaska with the most advanced technology and unsurpassed expertise to manage and treat all types of breast cancer.
Breast cancer can begin in different areas of the breast — the ducts, the lobules, or in some cases, the tissue in between. In this section, you can learn about the different types of breast cancer, including non-invasive, invasive, recurrent, and metastatic breast cancers. You can also read about breast cancer in men.
The most common types of invasive breast cancer are:
There are two types of breast tumors that are non-invasive, meaning they have not invaded through the wall of mammary gland duct or lobule. These types of cancer are almost 100% curable when properly treated. They are precursors to their invasive counterparts:
Breast cancer in men is very rare, but approximately 2,600 men are expected to be diagnosed this year. A number of factors can increase the risk of breast cancer in men, including:
The most common classification for staging breast cancer is the American Joint Committee on Cancer (AJCC) 8th edition TNM classification system. There are many sub-types of categories It features:
TNM status are grouped to create an overall stage. There are many sub-categories of overall stage. It essentially can be summarized by 5 groups:
When breast cancer is found early, the success rate is nearly 100%. The American Cancer Society recommends breast screenings annually for women over 45 and continuing as long as you are in good health. Other organizations, including the Mayo Clinic and your radiology oncologists at Mat-Su Valley Cancer Center, suggest you begin annual screenings at age 40. In women with a strong family history of breast cancer breast screening should begin by age 35 or younger.
The staff of caring and qualified radiologists can determine the best type of imaging for your needs including:
The majority of breast cancers are managed with surgery. Most women, 80-90%, have the option of having the breast removed or just the cancer itself. For women who choose to keep their breast, radiation therapy is recommended to minimize the risk of cancer returning in the breast or surrounding tissue. The cure rates for total breast removal, known as a mastectomy, and partial breast removal (aka lumpectomy) followed by radiation therapy are equal. While surgery and radiation therapy are local treatments, systemic therapy is often recommended. Systemic therapy can involve chemotherapy, immunotherapy, or anti-estrogen therapy. Your medical oncologist will assist in making an informed decision regarding systemic therapy. When it comes to treating your breast cancer with radiation therapy, Mat-Su Valley Cancer Center is your radiation oncologists choice.
Our oncologists are experienced in all forms of cancer, including:
Cancer is never something you want to hear about or deal with. It is sometimes too scary to even say out loud sometimes. Let Mat-Su Valley Cancer Center help alleviate some of your concerns by answering the most frequently asked questions about breast cancer for you.
The professional advice for this question has changed in recent years. The American Cancer Society recommends annual mammography screenings for all women when they turn 45 years old. Other prominent organizations, including the Mayo Clinic and our Mat-Su Valley Cancer Center specialists, suggest you begin annual screenings at age 40. Women at higher risk should begin screening no later than age 35.
If your radiologist finds something suspicious in your mammogram scan, he or she will order additional screenings to confirm whether you have an abnormal group of cells that has formed a tumor. Once that is confirmed, they may take a biopsy of the tissue to test whether it is cancerous (malignant) or benign. Mat-Su Valley Cancer Center will work with your primary care physician to confirm the diagnosis and develop an individualized cancer treatment plan for you.
When detected early, cancer survival rates are excellent. Many factors influence an individuals likelihood of success.
Women who do regular monthly exams as recommended may notice a change in the shape or size of lump in their breast. Others have no symptoms and find out during their annual mammogram when a radiologist spots a clump of abnormal cells. Check out our Breast Cancer – Detection & Treatment Options page for more information.
There are many risk factors connected with the development of breast cancer. However, the links between these factors and women who develop breast cancer is still unclear. Besides being a woman and getting older, hormone levels seem to play a major part in the development of breast cancer, but it is not clear to what extent.
Cells become cancerous in a woman’s breast when her DNA is changed or mutated. DNA is complex molecule that carries the information that makes a living organism function. It is the chemical in our body that makes up our genes, which can tell our cells when to grow, divide or die. Sometimes these mutations are inherited. But oftentimes, your DNA is changed throughout your life, possibly through prior exposure to radiation therapy or cancer-causing chemicals.
While you cannot control your family history, other lifestyle choices you can control are shown to increase your risk of breast cancer, including:
Fortunately, few women diagnosed with breast cancer require mastectomy, or removal of the breast. Almost all women diagnosed with breast cancer, however, have the option of mastectomy with or without immediate reconstruction. Many women who have a non-invasive tumor select the option of a lumpectomy to remove the tumor, followed by radiation therapy to help prevent recurrence of any cancer.
Because there are so many stages and types of breast cancer, the treatment options also vary. Mat-Su Valley Cancer Center offers the most comprehensive array of radiation therapy. Check out the detailed treatment options available to you.
High doses of radiation therapy are used to kill cancer cells during cancer treatment. This radiation therapy can also affect surrounding tissue and organs. Because of the advanced technology at Mat-Su Valley Cancer Center, the damage to surrounding tissue is greatly minimized with fewer side effects. However, general side effects from radiation therapy include fatigue and skin irritations (itching, peeling, dryness, redness) at the site of the radiation therapy.
Contact us at Mat-Su Valley Cancer Center at 907-707-1333. We are here to explain the variety of treatment options available to you and make sure all of your questions are answered. For your convenience, we also have an online contact form that you may use to ask your questions or make your first appointment. Your first phone consultation is free, so don’t hesitate to give us a call today. You owe it to yourself to explore all treatment options available to you.