


Your liver serves an important function: to filter out waste and toxins from the bloodstream and prepare those for excretion. The liver is such a vital organ – and being largest organ inside your body – you cannot live without it. Any sign of a tumor presenting itself on your liver should be examined closely at Mat-Su Valley Cancer Center to determine what you are dealing with and how to treat it. The sooner you act on the presence of a liver tumor, the better.
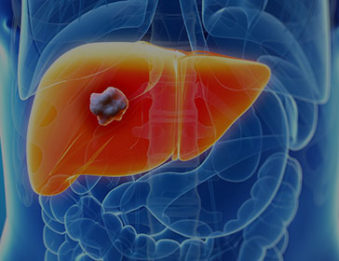 There are two ways that tumors can appear in the liver: they either travel there from another part of the body or grow in the liver from the start. Tumors that travel from elsewhere in the body are known as metastatic tumors. They are secondary tumors that can get into the liver via the bloodstream. Metastatic tumors could indicate a serious issue stemming from another part of the body and require a thorough inspection to form a treatment plan.
There are two ways that tumors can appear in the liver: they either travel there from another part of the body or grow in the liver from the start. Tumors that travel from elsewhere in the body are known as metastatic tumors. They are secondary tumors that can get into the liver via the bloodstream. Metastatic tumors could indicate a serious issue stemming from another part of the body and require a thorough inspection to form a treatment plan.
Tumors that originate in the liver are known as primary tumors. Some may be benign, or noncancerous, but others could be cancerous and require aggressive treatment. While liver cancer accounts for up to half of cancer diagnoses in undeveloped countries, it is relatively rare in the United States, accounting for about 2 percent of cancers. The average age for those diagnosed with liver cancer is about 67 in the U.S. Men are two times more likely to contract liver cancer than women.
One of the first steps following the detection of a liver tumor is to quickly ascertain the type of tumor it is. If it is benign, no further action is necessary other than regular health monitoring. If the tumor is cancerous, then it is imperative that your medical professional identify the stage, which will help to determine how far the cancer has spread and which treatment option is best for fighting it.
Primary liver tumors are those that originate or start in the liver. They don’t travel from another part of the body to the liver. There are two types of primary liver cancer tumors: hepatocellular carcinoma and cholangiocarcinoma.
Hepatocellular carcinoma is more commonly referred to as HCC, and it’s by far the most common type of liver cancer diagnosed. This cancer can occur due to cirrhosis of the liver. Risk factors can include
Cholangiocarcinoma, which is also known as bile duct cancer, is much rarer than HCC, and it is also much more difficult to treat due to how quickly it advances.
When determining stages for Anchorage liver tumor treatment, your physician will look at size (T), spread (N), and metastasis (M) of the tumor. The tests will place a number next to each of these letters – if an X appears, it means that particular aspect couldn’t be assessed. Stage 0 means there is no tumor, it has not spread, or it has not metastasized to other parts of the body. Your physician will combine the numbers to ascertain the stage of any cancerous tumors, which will use Roman numerals to number it 1 to 4, with 4 being the most advanced.
The detection of a liver tumor can sometimes be difficult without the assistance of the qualified Mat-Su Valley Cancer Center. This is because cancerous tumors might not present any symptoms in the early stages. Once the cancer advances far enough, individuals may start to experience pain in the upper right abdomen where the liver is located. Sudden weight loss, loss of appetite, and yellowing eyes and skin – an indication of jaundice – could also be symptomatic of liver cancer. Your physician will want to perform a few tests to find out if that is what you are dealing with.
Your radiation oncologist will likely order a combination of tests in order to ensure an accurate diagnosis. The most common detection methods include
Every cancer case is unique, so if you receive a diagnosis of liver cancer, your oncologist will likely work with you to come with a treatment plan tailored to your needs and the stage of your cancer. Every treatment option has its advantages and drawbacks, so you will want to thoroughly explore all of your options and even get a second opinion. Don’t be afraid to ask your physician questions about anything – after all, we are here to help you win this battle. Some treatment options you are likely to hear include
Our comprehensive cancer center is fully staffed with oncologists who specialize in:
The liver is the largest solid organ in the body. It is located behind the ribs on the right side of the body, under the right lung. It is important for many metabolic functions.
No. The liver stores nutrients that help feed the body when a person has not eaten for a few hours. It also changes other nutrients into more basic elements before sending them to other parts of the body to be used. The liver helps break down sugars, starch, fats, and proteins.
The liver also makes albumin, a protein that helps the body balance fluids. The liver makes clotting factors. They help blood thicken or clot when a person is bleeding. Bile made in the liver is important for digesting food and for other bodily functions.
One of the liver’s most important functions is to collect and destroy poisons in the body. The liver breaks down and removes medicines. When the liver is not working well, chemicals can build up inside the body and cause damage.
Liver cancer is cancer that starts in the cells of the liver. It is not the same as cancers that start somewhere else in the body and then spread to the liver. Healthcare providers call those cancers liver metastases (or secondary liver cancers).
Liver cancer is rare in the United States and Europe. It is the most common form of cancer in some African and East Asian countries, though. There are several kinds of liver cancers:
Approximately 40,000 cases of liver cancer are diagnosed each year. Men are more likely to get liver cancer than women.
A person can have liver cancer for months or years before having symptoms of the disease. People do not usually show symptoms of liver cancer until the cancer grows large enough to push against other parts of the liver or against other organs in the stomach.
People with liver cancer may have any or all of these symptoms:
All these symptoms can be caused by many other medical problems. If you have any of these symptoms, you should see your healthcare provider as soon as possible.
If you think you might have liver cancer, you should have a medical exam. Many tests may be needed to confirm liver cancer. The steps to diagnosing liver cancer might include a medical history, physical exam, blood tests, imaging tests, and a liver biopsy (removing small pieces of tumor for lab tests). Imaging tests for liver cancer can include ultrasound, MRI (magnetic resonance imaging) and CT (computed tomography) scan. In some cases, the diagnosis of liver cancer can be made by MRI alone (without a liver biopsy). If the diagnosis is in doubt, however, a biopsy is performed.
Many people with cancer get an opinion from a second healthcare provider who is a liver specialist. There are many reasons to get a second opinion. Here are some of those reasons:
Many people have a hard time deciding on a liver cancer treatment. It may help to have a second healthcare provider review the diagnosis and treatment choices before starting treatment. It is important to remember that in most cases, a short delay in treatment will not lower the chance that it will work. Some health insurance companies even require that a person with cancer seek a second opinion. Most other insurance companies will pay for a second opinion if asked.
There are many ways to get a second opinion:
You may have one treatment or many treatments together:
Healthcare providers are always finding new ways to treat liver cancer. These new methods are tested in clinical trials. Before beginning treatment, you should ask your healthcare provider if there are any clinical trials you should consider.
Here’s an overview of some new prevention and treatment methods being studied:
Clinical trials are studies of new cancer treatments. Healthcare providers do clinical trials to learn how well new treatments will work. They also do trials to test for side effects. A promising treatment is compared to the current treatment to see if it works better or has fewer side effects. People who participate in these studies may benefit from new treatments before the FDA approves them. Research studies also help further our understanding of cancer and help future cancer patients.
If all of these types and stages of liver cancer are confusing to you, give the experts at Mat-Su Valley Cancer Center a call at 907-707-1333. We are here to explain the variety of treatment options available to you and make sure all of your questions are answered. For your convenience, we also have an online contact form that you may use to ask your questions or make your first appointment. Your first phone consultation is free, so don’t hesitate to give us a call today. You owe it to yourself to explore all treatment options available to you.